Science and technology
科學技術
Embryonic stem cells
胚胎干細胞
Looking up
進展中的干細胞研究
Stem-cell research is now bearing fruit
干細胞研究開始結出碩果
FOURTEEN years ago James Thomson of the University of Wisconsin isolated stem cells from human embryos.
十四年前,當威斯康辛大學的 James Thomson從人類胚胎細胞中分離出干細胞時,
It was an exciting moment.
人們無不為之歡呼雀躍。
The ability of such cells to morph into any other sort of cell suggested that worn-out or damaged tissues might be repaired,
這種細胞可分裂、轉變成為各種器官、組織,因此或將被用于修復、
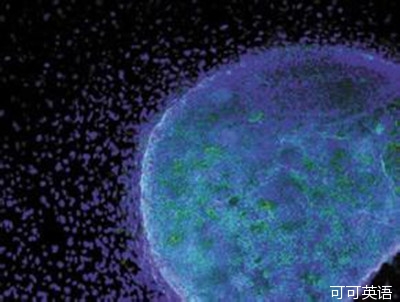
and diseases thus treated a technique that has come to be known as regenerative medicine.
治療損傷、病變的組織,這一技術被稱為再生醫療。
Since then progress has been erratic and controversial.
但隨后這一領域的發展呈現了不穩定性、胚胎細胞的來源問題也引發了社會爭議。
But, as two new papers prove, progress there has indeed been.
但是這兩篇新論文的發表,證明了干細胞研究取得了一定的進展。
This week's Lancet published results from a clinical trial that used embryonic stem cells in people.
本周《柳葉刀》刊出了胚胎干細胞應用于人體的臨床實驗的結果。
It follows much disappointment.
人們對這樣的消息常常都是失望:
In November, for example, a company in California cancelled what had been the first trial of human embryonic stem cells, in those with spinal injuries.
例如,去年11月,一家位于加州的公司取消了原定的首例人胚胎干細胞在脊髓損傷者身上的試驗。
Steven Schwartz of the University of California, Los Angeles, however, claims some success in treating a different problem: blindness.
但是洛杉磯加州大學的Steven Schwartz說他在干細胞治療其它疾病:如失明,就取得了一些成績。
His research, sponsored by Advanced Cell Technology, a company based in Massachusetts, involved two patients.
他的研究是在先進細胞技術院的贊助下進行的,這家公司位于馬薩諸塞州,兩名病患參與了試驗,
One has age-related macular degeneration, the main cause of blindness in rich countries.
一位是老年性黃斑變性病患者,這是發達國家盲人病患常見的致盲原因。
The other suffers from Stargardt's macular dystrophy, its main cause in children.
另一位是隱性黃斑營養不良癥患者,這是兒童致盲的主要原因。
Dr Schwartz and his team coaxed embryonic stem cells to become retinal pigment epithelium tissue which supports the rod and cone cells that actually respond to light
他的團隊誘導胚胎干細胞成為視網膜色素上皮組織細胞-其中的桿細胞及錐晶細胞對光線敏感。
then injected 50,000 of them into one eye of each patient,
然后給每個參試病患的眼睛內注射50,000單位的此種細胞,
with the hope that they would bolster the natural supply of these cells.
希望這些細胞能在體內像原有細胞一樣自然生長。
The result was a qualified success.
結果相當成功。
First and foremost, neither patient had an adverse reaction to the transplant always a risk when foreign tissue is put into someone's body.
首先,也是最重要的是,兩位病患都沒有對新移植的細胞產生排斥-這是移植異體組織常常要面臨的風險。
Second, though neither had vision restored to any huge degree, each was able, four months after the transplant,
其次,雖然兩名患者的視力沒有很大程度的恢復,但移植4個月后,
to distinguish more letters of the alphabet than they could beforehand.
與患病前相比,他們都能識別出更多視力表上的字母了。
Whether Dr Schwartz's technique will prove truly useful remains to be seen. Experimental treatments fail far more often than they succeed.
但現在就確定的說Dr Schwartz的技術很實用還為時尚早,失敗的試驗遠比成功的案例更多。
But the second paper, published in Nature by Lawrence Goldstein of the University of California, San Diego, and his colleagues,
但由圣迭戈加州大學的 Lawrence Goldstein及其同事發表在《自然》雜志的這篇論文,
shows how stem cells can be of use even if they do not lead directly to treatment.
也是我想說的第二篇論文,就能看出干細胞盡管還不能直接用于治療,但已經相當“好使”了。
Since 2006 researchers have been able to reprogram adult cells into an embryonic state, using proteins called transcription factors.
自從2006年以來,研究人員已經能用一種稱為轉錄因子的蛋白質分子將體細胞誘導成為類似胚胎細胞的干細胞,
Though these reprogrammed cells, known as induced pluripotent stem cells, might one day be used for treatment,
盡管這種誘導多潛能干細胞遲早會有一天能在再生醫療領域大展拳腳,
their immediate value is that they are also an excellent way to understand illness.
但眼下,它們的價值則體現在對疾病的研究上,這是個很好的方法。
Using them, it is possible to make pure cultures of types of cells that have gone wrong in a body.
利用它們就能離體培養出與體內患病組織相同類型的細胞來。
Crucially, the cultured cells are genetically identical to the diseased ones in the patient.
關鍵是,這些培養出的細胞與患者的染病細胞在基因組成上是相同的。
Dr Goldstein is therefore using iPS cells to try to understand Alzheimer's disease.
因此,Dr Goldstein將用iPS來揭開阿爾茨海默癥的病因。
The brains of those with advanced Alzheimer's are characterised by deposits,
重癥阿爾茨海默病患者的大腦內明顯特征是,有一種稱為淀粉樣蛋白碎片的積淀物,
known as plaques, of a protein-fragment called beta-amyloid, and by tangles of a second protein, called tau.
也是我們所稱的斑塊,與另一種蛋白的結團物。
But how these plaques and tangles are related remains unclear.
但這些斑塊和結團是何種關系還不明確。
To learn more, Dr Goldstein took tissue from six people:
為了深入研究, Dr Goldstein從6位病患身上取了組織:
two with familial Alzheimer's, a rare form caused by a known genetic mutation;
2位是家族阿爾茨海默病患者-因較罕見的基因突變所引發的;
two with sporadic Alzheimer's, whose direct cause is unknown; and two unaffected individuals who acted as controls.
2位是散發性阿爾茨海默病患者-致病原因不詳;2位是行動可控的未患病者。
He reprogrammed the cells collected into iPS cells, then nudged them to become nerve cells.
先將收集的體細胞誘導成iPS,再用這些iPS細胞轉化神經細胞。
In three of the four Alzheimer's patients these lab-made nerve cells did,
4位阿爾茨海默病患者中,3位的實驗獲得神經細胞中,表現出高水平的淀粉樣蛋白和蛋白,
indeed, show higher levels of beta-amyloid and tau and also of another characteristic of the disease, an enzyme called active GSK3-beta.
并且,與此疾病相關的另一特征:一種稱為GSK3活性酶的水平也較高。
Since he now had the cells in culture, Dr Goldstein could investigate the relationship between the three.
于是,他將這三種神經細胞植入培養皿中培養,以發現三者之間的關系。
To do so he treated the cultured cells with drugs.
之后,他就能用藥物來處理培養出的細胞。
He found that a drug which attacked beta-amyloid directly did not lead to lower levels of tau or active GSK3-beta;
他發現用藥物直接處理淀粉樣蛋白并不能致使Tau蛋白和GSK3活性酶的水平降低;
but a drug which attacked one of beta-amyloid's precursor molecules did have that effect.
但如果用藥物處理淀粉樣蛋白的前體分子,效果就會很好。
That is useful information, for it suggests where a pharmacological assault on the disease might best be directed.
這是很有價值的信息,能判斷在哪里用藥才能直達病灶。
In the short term, at least, iPS-based studies of this sort are likely to yield more scientific value than clinical experiments of the type conducted by Dr Schwartz,
在短期內,此類基于iPS的研究在科學價值方面的意義遠大于Dr Schwartz進行的臨床實驗結果,
even though they are not treatments in themselves.
因為他們的研究本身還不能用于治療病患。
That will, though, require many more pluripotent cells.
不過,對多潛能干細胞的需求會與日俱增,
And at least one firm is selling a way to make billions of iPS cells for just that purpose.
至少有一家公司會源源不斷的提供數十億的iPS細胞用于此類研究,
Its founder, appropriately, is Dr Thomson.
它的創始人正是Thomson.